Reassurance about the benign nature of Autonomic Mediated Syncope (Neurocardiogenic Syncope, Vasovagal Syncope), avoidance of situations likely to induce an attack, and use of simple non-drug counter-measures is often all that is required in the management of the condition. However, treatment with low dose medication may be necessary. Occasionally pacemaker implantation may be required.
Recommended non-drug measures
• Avoid situations likely to induce syncope – for example, standing in a queue, taking a long hot bath, eating a large carbohydrate-rich meal in a warm restaurant, or failing to drink sufficient fluid in a hot nightclub.
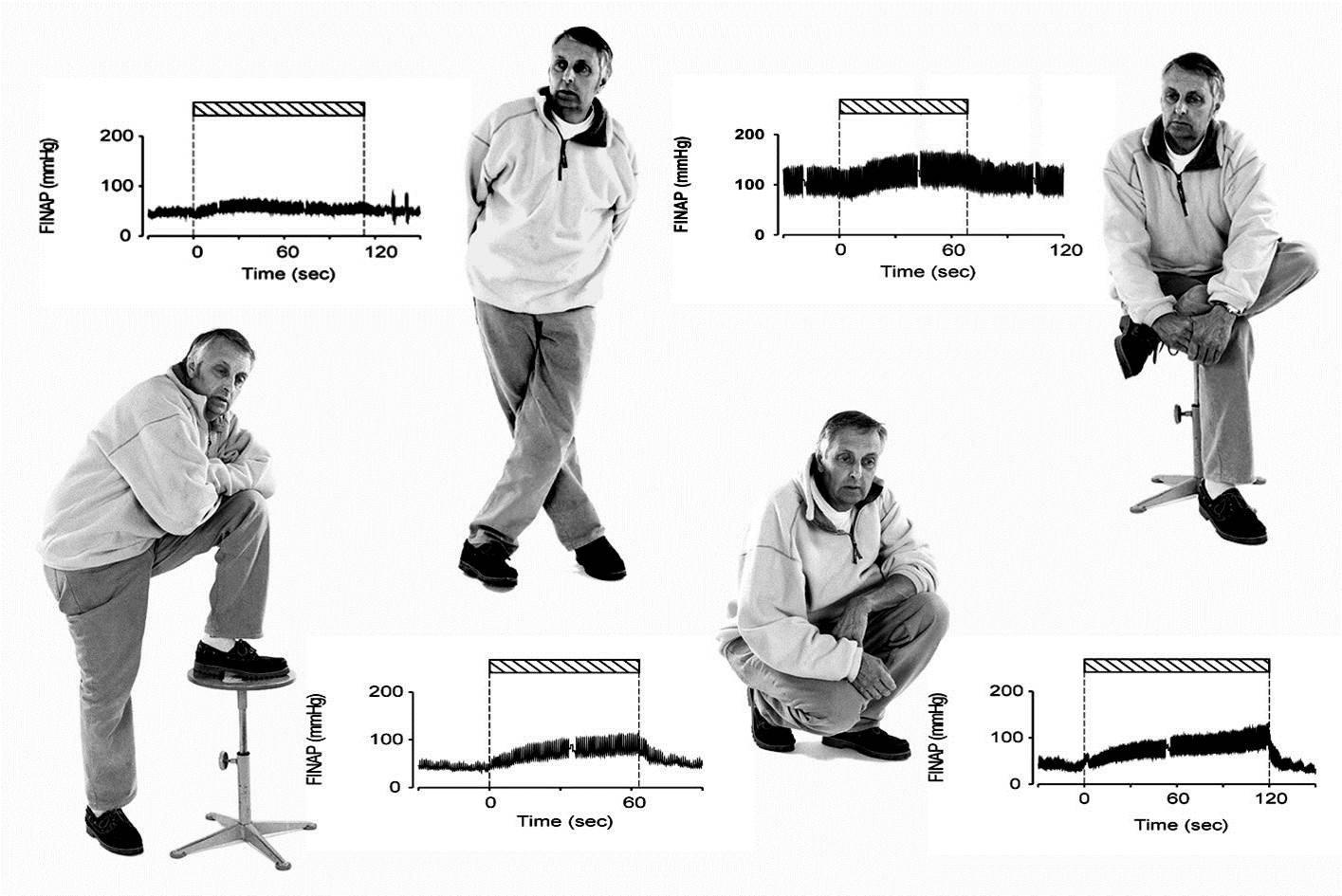
• Take immediate action at the first warning of an impending collapse. If a collapse is imminent lie down flat propping your legs up on a chair or against a wall or sit down with your head between your knees. Squatting down on ones heels can be very effective and is less likely to attract attention in public . All these manoeuvres help reverse venous pooling of blood in the limbs, swiftly restoring blood flow to the brain and alleviating symptoms. When sufficiently recovered get up carefully. If your symptoms return or worsen squat down, or lie down again.
• Compression stockings can reduce venous pooling in the legs. Compression socks are not very effective, and full length stockings fall down, so compression tights are the best option. In the UK compression garments, including tights for both males and females, can be dispensed on prescription by your GP. For detailed information on compression tights available on the NHS, please see here.
• Our experience is that abdominal binders are at least as effective as compression stockings, and are much easier to put on. There are several brands available to buy. Having tried a number of them on patients our current favourite is this one. These work by reducing splanchnic venous pooling in the abdomen.
• Drink 200 mls of water. This promptly increases blood pressure in normal subjects and in patients with autonomic failure. It may also be helpful in preventing vasovagal syncope. Ensuring adequate intake, as determined by the clear appearance of urine, may help prevent collapses.
• Increase your dietary intake of salt if your oral intake is low – 24 hour urinary sodium excretion is a proxy measure. This may be achieved by adding salt at the table, taking salt tablets (Slow Sodium) or drinking “sport” drinks. Up to 12 g of salt per day may be required – equal to 20 Slow Sodium tablets, each of which contain 600 mg of salt (232 mg of sodium). That is equivalent to 4.6 g of sodium. A level teaspoonful contains 5 g of salt, which is equivalent to 2 g of sodium. The benefits from increasing salt intake are noticed within two or three days. You should not increase your salt intake if you have hypertension – high blood pressure.
• Sleep with the head of your bed raised by about 10°. This reduces urinary salt loss overnight.
• Endurance training can be helpful if you are not fit. Using a rowing machine is an excellent form of exercise and may reduce your tendency to collapse.
• Tilt table training has been used successfully, but needs to be maintained as deconditioning occurs rapidly on cessation.
Pharmacological treatment
Various medications have been used to treat Autonomic Mediated Syncope (Neurocardiogenic Syncope, Vasovagal Syncope).
Beta blockers (Antihypertensive and antianginal drugs) such as Bisoprolol at low dose can be effective. These drugs may act by preventing the inappropriate activation of the stretch receptors in the left ventricular muscle.
Fludrocortisone (a mineralocorticoid used to treat low blood pressure) increases blood pressure by reducing urinary sodium and water loss. This minimises the effects of venous pooling in the legs.
Small doses of an SSRI (Selective Serotonin Re-uptake Inhibitors used to treat depression) such as Fluoxetine (Prozac) or Paroxetine (Seroxat) can be effective. It is thought that serotonin helps regulate stretch receptor activation.
Midodrine (a vasoconstrictor) acts by constricting the arterioles that control blood pressure. This action raises blood pressure.
Disopyramide (anti-arrhythmic drug) minimises vagotonic reflex slowing of the heart.
If one drug is not effective, it is always worthwhile trying one of the others from a different class.
Many of the clinical trials that showed benefit from treatment were not placebo-controlled. Results from the few placebo-controlled trials that have been carried out so far have generally been disappointing. SSRIs and Midodrine currently have the strongest scientific evidence.
The fact that so many different medications are used in the treatment of Autonomic Mediated Syncope (Neurocardiogenic Syncope, Vasovagal Syncope) indicates that none is entirely effective. Sometimes, a combination of drugs is required.
Abolition of symptoms indicates successful treatment. Although the Tilt Table Test may be rendered negative, repeating the test on treatment is not a good indicator of success and is not recommended.
Medication should be reduced once symptoms have been abolished for a year or so. If symptoms do not recur as the dose is reduced, then the medication may be discontinued.
Pacemakers
Occasionally permanent pacemaker implantation is necessary – generally when tilt table testing elicits prolonged cardiac standstill.
Scientific medical opinion is still divided about the role of pacemakers in vasovagal syncope. Ongoing research should help clarify the situation.