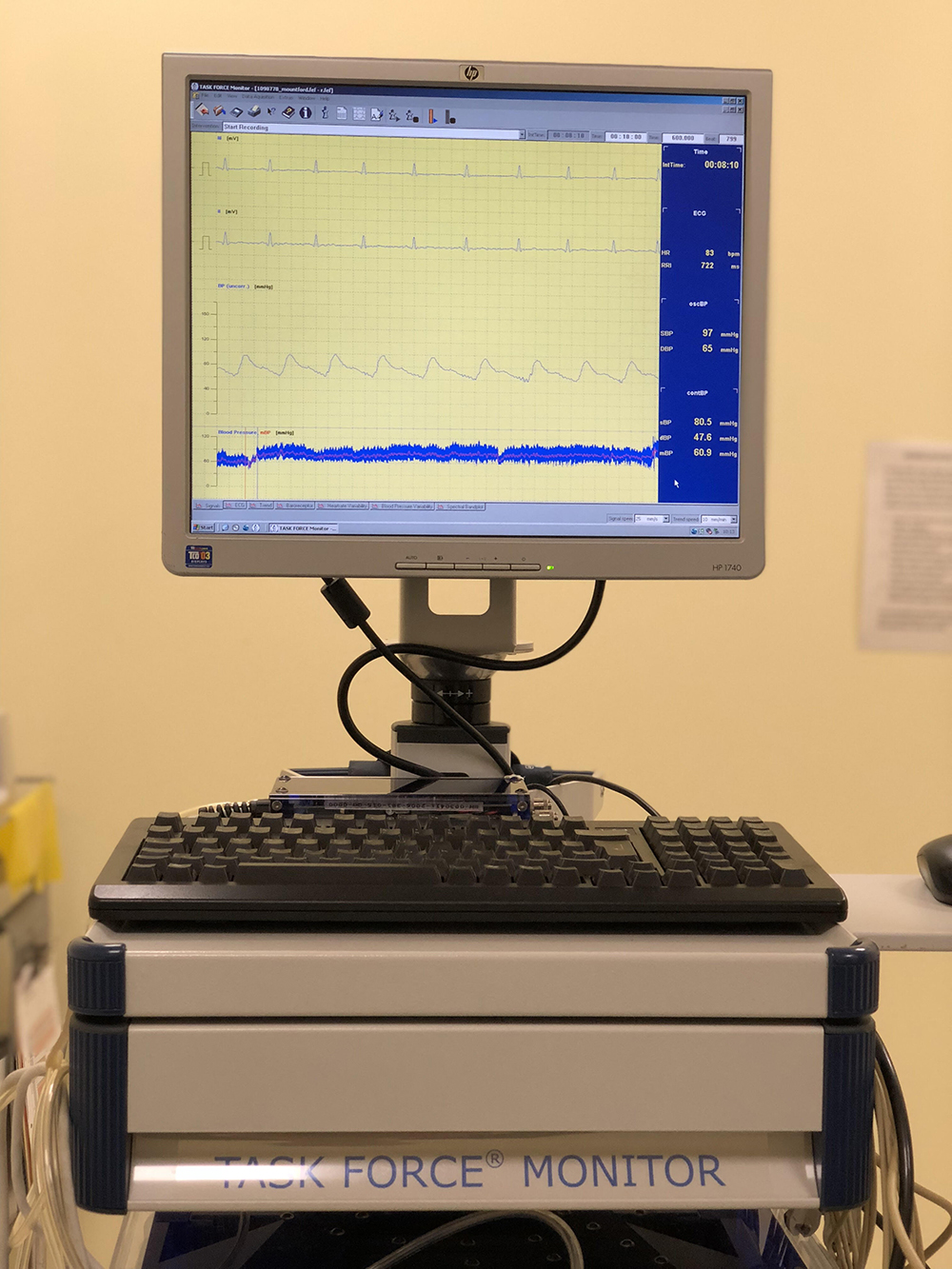
A Tilt Table Test is performed in a quiet warm room specially equipped for the investigation. The individual lies flat on a tilt table and is attached to real-time ECG and blood pressure monitoring equipment. After a short period of rest the table is tilted (head up) to 70° and maintained at that angle for 40 minutes or until typical symptoms occur. 50% to 60 % of patients with unexplained syncope reproduce their symptoms at around 20 minutes, often with associated dramatic slowing of the heart rate or even ventricular standstill – see NCS bradycardia and NCS asystole – and precipitous lowering of the blood pressure – see graphs.
The exact pattern of the heart rate and blood pressure change can help determine the best line of treatment. Removing the tilt restores the heart rate and blood pressure to normal and quickly abolishes symptoms. The sensitivity of the test may be increased by administering Glyceryl Trinitrate 400 micrograms (Nitrolingual Spray ) 20 minutes into the test, continuing for another 20 minutes or until typical symptoms/syncope occur.
Currently trials are testing the specificity and sensitivity of Glyceryl Trinitrate 800 micrograms administrated 10 minutes before tilting, followed by tilting at 70° for 20 minutes or until typical symptoms/syncope occur.
Induced syncope is much more common when Glyceryl Trinitrate is used. It is therefore essential to demonstrate slowing of the heart rate at the point of syncope before concluding that the collapse is due to Autonomic Mediated (Neurocardiogenic) syncope.
Glyceryl Trinitrate should not be used in Aortic Stenosis, HOCM, Mitral Stenosis, Constrictive Pericarditis, Pulmonary Hypertension, Anaemia or Hypovolaemia.
Patient Presenting Charts
These traces show the typical changes in systolic blood pressure and heart rate induced during a positive tilt table test.
Fifteen minutes into the test the BP (upper trace) fell precipitously from 140 mm Hg to 50 mm Hg and the heart rate (lower trace)
dropped from 65 beats per minute to 30 beats per minute. The patient developed typical symptoms.
Removing the tilt resulted in rapid recovery.
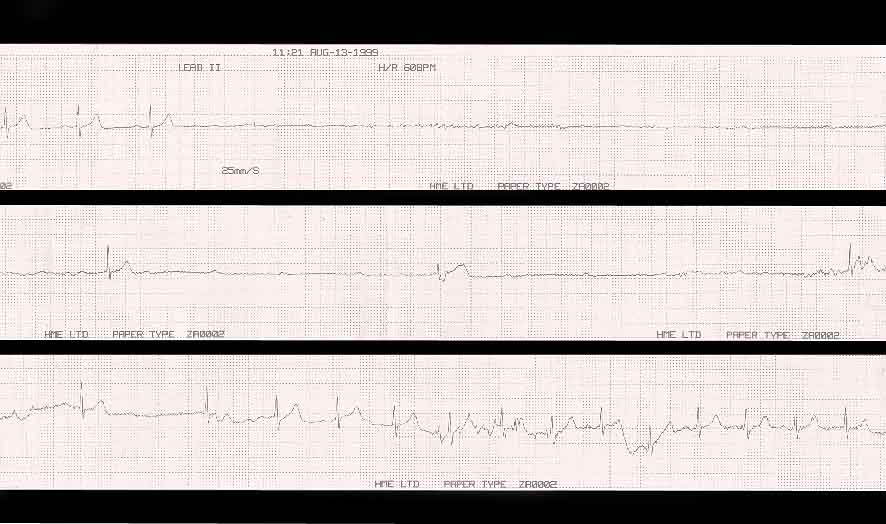
This patient had a history of passing out. In this case the blood pressure dropped steadily from the onset of the tilt table test. The initial systolic BP of 155 mm Hg dropped to 60 mm Hg over 30 minutes, associated with an increase in heart rate from 85 beats per minute to 100 beats per minute.
The patient felt rather light-headed at this stage!
20 minutes into the test both systolic blood pressure and heart rate are steady. Following 400 mcg of sublingual GTN the heart rate rose swiftly from 80 beats per minute to 140 beats per minute while the systolic blood pressure fell from 80 mmHg to 30 mmHg at the point of syncope.
The test is negative because there was insignificant (<20%) drop in heart rate following profound GTN induced hypotension.
On lying the patient flat the blood pressure swiftly recovered and the heart rate returned to normal.
20 minutes into the test both systolic blood pressure and heart rate are steady. Following 400 mcg of sublingual GTN the heart rate rose from 90 beats per minute to 150 beats per minute while the systolic blood pressure drifted down from 110 mmHg to 80 mmHg. The heart rate then suddenly dropped to 80 beats per minute accompanied by a swift fall in systolic blood pressure to 20 mmHg at the point of syncope.
The patient experienced his usual symptoms prior to blacking out. He made a quick recovery on lying flat.
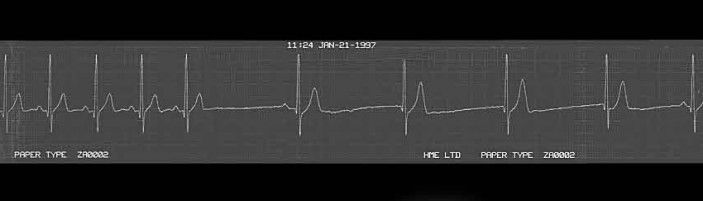
Sometimes the vagotonic tone induced by Autonomic Mediated Syncope is so intense that prolonged ventricular standstill ensues. This may cause hypoxic syncopal convulsions.
This patient had a history of dramatic collapses.
The ECG trace shows ventricular standstill of 16 seconds followed by one ventricular contraction and then another 13 seconds without an effective contraction. Ventricular activity then resumed spontaneously.
Following diagnosis he was fitted with a pacemaker and has been asymptomatic since.
QUICK ENQUIRY